Pelvic fractures are often underestimated because the pain may seem mild or diffuse, yet these injuries can have serious consequences if left undiagnosed. Unlike hip fractures, pelvic fractures can affect surrounding nerves, blood vessels, and organs, making early recognition critical. Understanding the subtle and overt signs—beyond obvious trauma—empowers adults 40–70 to seek prompt evaluation, prevent complications, and protect long-term mobility, ensuring recovery is safe, effective, and supported by appropriate orthopedic care.
Understanding Pelvic Fractures
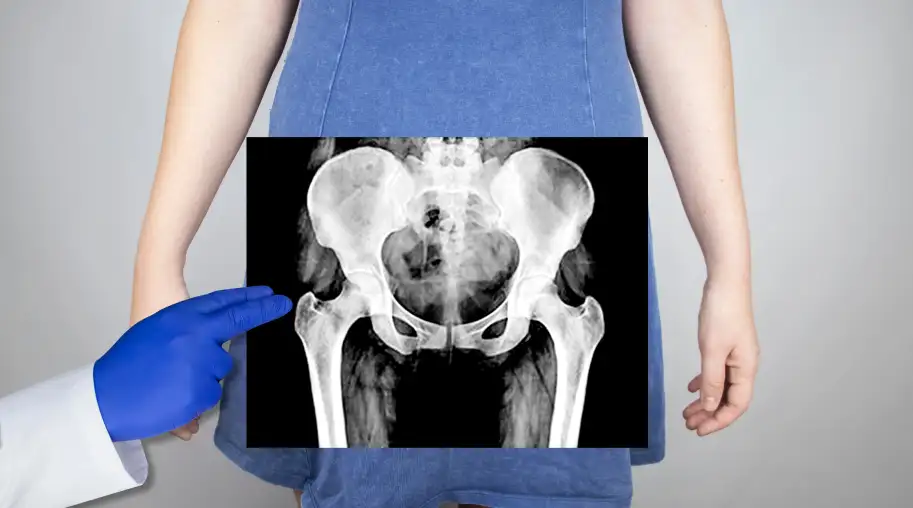
A pelvic fracture occurs when one or more bones in the pelvis—such as the iliac bones, pubic rami, or acetabulum—break or crack. What many patients don’t realize is that the pelvis is a ring-like structure, so a fracture in one area can compromise stability elsewhere. Pelvic fractures vary widely in severity: some are stable and can heal with rest, while others are unstable and require surgery due to the risk of internal bleeding or organ injury. Unlike hip fractures, pelvic fractures may not always cause immediate, sharp pain, making subtle symptoms like groin discomfort, difficulty walking, or changes in bladder or bowel function essential clues for early detection.
Common Causes and Risk Factors
Pelvic fractures can occur in a variety of situations, and some risk factors are often overlooked. Understanding these causes helps adults 40–70 recognize when to seek prompt evaluation.
- Traumatic Injuries: High-impact events like car accidents, falls from a height, or sports collisions can fracture pelvic bones, even in otherwise healthy adults.
- Low-Energy Falls in Older Adults: For adults with decreased bone density or osteoporosis, even a minor trip or fall from standing height can lead to a fracture.
- Osteoporosis and Bone Weakness: Age-related bone loss makes the pelvis more vulnerable to fractures from both minor trauma and everyday activities.
- Chronic Hip or Pelvic Pain: Pre-existing conditions can alter gait and load distribution, increasing stress on the pelvic bones.
- Lifestyle and Activity Factors: Sedentary behavior, poor nutrition, or vitamin D deficiency can weaken bones over time.
- Medical Conditions: Diseases such as cancer, rheumatoid arthritis, or prolonged corticosteroid use can compromise bone integrity.
Recognizing these causes and risk factors early allows patients and caregivers to be vigilant, seek timely evaluation, and reduce the likelihood of complications that can arise from missed or delayed diagnosis.
Diagnosis and Evaluation
Diagnosing a pelvic fracture requires careful evaluation because symptoms can be subtle, especially in older adults or low-impact injuries. Physicians begin with a detailed medical history and physical examination, assessing pain location, mobility limitations, and any signs of internal injury. Imaging is critical: X-rays provide an initial overview, while CT scans or MRI may be needed to identify complex fractures, assess joint involvement, or detect associated soft tissue damage. In some cases, blood tests or monitoring vital signs help detect internal bleeding. Early and accurate evaluation ensures proper treatment planning, whether non-surgical or surgical, and helps prevent complications such as nerve injury, chronic pain, or long-term mobility issues.
Signs and Symptoms to Watch For
Pelvic fractures can present with both obvious and subtle symptoms, making vigilance critical—especially for adults 40–70. Some warning signs are easy to overlook, yet recognizing them early can prevent complications:
- Localized Pain: Sharp or persistent pain in the groin, hip, lower back, or pelvic region, often worsening with movement or weight-bearing.
- Swelling and Bruising: Visible swelling, discoloration, or tenderness around the pelvic area, hips, or lower abdomen may indicate bleeding or tissue trauma.
- Difficulty Walking or Bearing Weight: Patients may limp, shuffle, or avoid putting pressure on the affected side, even after a minor fall.
- Changes in Hip or Pelvic Alignment: One leg may appear shorter or rotated, or the pelvis may feel unstable.
- Numbness or Tingling: Nerve involvement can cause tingling, weakness, or numbness in the thigh, groin, or lower leg.
- Bladder or Bowel Issues: Difficulty urinating, blood in urine, or constipation can signal internal involvement, which requires urgent attention.
- Subtle Functional Changes: Reduced ability to climb stairs, rise from a chair, or perform routine movements may indicate a fracture even without severe pain.
Awareness of these symptoms helps patients and caregivers seek prompt evaluation, enabling early intervention and reducing the risk of long-term complications.
Recovery and Rehabilitation
Recovery from a pelvic fracture is a gradual process that combines rest, mobility, and targeted rehabilitation. Stable fractures may heal with limited weight-bearing and guided physical therapy, while more severe or unstable fractures often require surgical repair followed by structured rehab. Early movement—such as gentle leg lifts, ankle pumps, and controlled range-of-motion exercises—supports circulation and prevents stiffness. As healing progresses, physical therapy focuses on strengthening the core, glutes, and hip stabilizers to restore balance and proper gait mechanics. Gradual reintroduction of weight-bearing activities, stair navigation, and functional movements ensures a safe return to daily life. Consistent monitoring of pain, swelling, and mobility during rehabilitation helps prevent setbacks and long-term complications.
Potential Complications and Warning Signs
While many pelvic fractures heal without long-term issues, certain complications can arise if the injury is missed or not properly managed. Internal bleeding is a serious risk, especially in unstable fractures, and can present as dizziness, rapid heart rate, or low blood pressure. Nerve damage may cause persistent numbness, tingling, or weakness in the legs. Improper healing can lead to chronic pain, pelvic instability, or leg length discrepancies, affecting mobility and daily function. Signs of infection, particularly after surgery, include redness, swelling, or fever. Early recognition of these warning signs, combined with prompt medical attention, is crucial to prevent lasting damage and support a safe, functional recovery.
Conclusion
Pelvic fractures can be serious injuries, and recognizing the signs early is essential for preventing complications and ensuring effective recovery. Pain, swelling, difficulty walking, or subtle functional changes should never be ignored, especially in adults 40–70 or those with risk factors like osteoporosis. Prompt evaluation, accurate diagnosis, and a tailored rehabilitation plan can make a significant difference in long-term mobility and quality of life. If you or a loved one suspect a pelvic fracture, don’t wait—visit SFHips or call (415) 530-5330 to schedule an appointment with our experienced orthopedic team and receive personalized care for your hip and pelvic health.